All ixodid ticks are temporary obligate ectoparasites, and a specific feature of their life cycle is multi-day feeding, during which the tick remains motionless at the site of its attachment on the host’s body. At this time, the parasite uses the body of its host not only for nutrition, but also as a genuine habitat.
At different stages of its development (larva, nymph, adult), the tick bites a suitable victim at least once - saturation with blood is a necessary condition for the further development of the body. At the same time, the tick is forced to periodically change from a free-living lifestyle to a parasitic one, and vice versa.
Despite these difficulties, ticks have many mechanisms of morphofunctional adaptation to this lifestyle, which makes them one of the most progressive groups of hemoparasites.
Lying in wait for a victim with a tick and attacking it
One of the most important events in the life cycle of a tick is when the hungry parasite finds a host on which to feed. How quickly a tick finds a victim and how completely it feeds on it determines its entire future life and partly the development of the species as a whole.
Therefore, the entire feeding strategy is to use the host as a source of nutrition as efficiently as possible. To do this, the tick very carefully selects hunting sites, prey, and, even more so, the place of attachment to it (after all, choosing the wrong place to bite means with a high probability of being discovered and killed).
On a note
It has been proven that behavioral reactions aimed at searching for prey are activated only in hungry ticks that have reached the so-called “state of aggressiveness.” In this state, the functioning of the tick's sensory organs and receptors is activated, and the parasite can effectively perceive stimuli emanating from the future victim.
Ticks have 2 types of searching and lying in wait for prey:
- passive lying in wait;
- active pursuit.
The passive method consists in lying in wait for the victim in places where they often gather (forest paths, pastures, parks and squares). Much less common is active pursuit, when the parasite, sensing the victim, begins to actively move in its direction, approaching it. However, this mechanism is conventionally called an attack - the tick does not attack a person or animal, and, contrary to popular belief, does not jump or fall from trees.
On a note
Active pursuit is used by ticks extremely rarely, since it requires increased energy expenditure and, in addition, when moving forward along heterogeneous surfaces, the parasite quickly loses moisture from the body. Therefore, after a short period of time of such a “hunt,” the tick is forced to stop pursuing and descend into the moist upper layers of soil or leaf litter, where absorption (absorption) of water through the integument of the body is possible.
The process of searching for a victim consists of two phases. The first phase is the spatial orientation of the tick. At this moment, the arthropod qualitatively evaluates all environmental factors (humidity, temperature, chemical composition of the air) and climbs to the most convenient place for itself, often on herbaceous vegetation, after which it settles in its upper tier.
The second phase begins when the tick senses the approach of the victim. At the same time, it turns its body towards the possible owner, extends the first pair of legs upward and makes oscillatory movements. At the ends of its legs there are sharp claws, with which the tick clings to the clothing or fur (feathers) of the victim.
On a note
Ticks do not have a specialized organ that would help them determine the position of the body relative to the ground, so the animal is oriented solely by the degree of tension of certain muscle groups of the limbs. When hunting, when the front legs are extended upward, the other three pairs hold the body in the desired position, performing both attachment and sensory functions. Therefore, purely anatomically, a tick cannot bend over a victim or fall onto it from a tree.
If, some time after the tick smells the host, contact does not take place, but stimuli continue to emanate, the parasite descends to the ground and begins to crawl towards the victim. This is a purely instinctive process - the incentives of the victim’s presence and hunger force the tick to resort to active actions, even if they are unprofitable from the point of view of physiology and energy consumption. But if the parasite does bite in, this will more than compensate for all the losses of energy and moisture during the hunt.
How do ticks sense their prey? First of all, in terms of the component composition of the air. The most powerful irritant is an increase in carbon dioxide levels. Other components released by the body of animals also have an effect, including hydrogen sulfide and ammonia.
The main distant chemoreceptor is Haller's organs, located on the forelimbs of ticks. They look like pits, at the bottom of which there is a cluster of sensitive cells. These cells perceive the slightest change in the concentration of the above substances and prompt the tick to act. The tick can sense a potential victim at a distance of more than 10 meters. This explains the massive accumulations of ticks in places where there are a large number of animals and people.
The question of whether ticks hear is still controversial. Soil vibration is certainly an irritant, but does not prompt the parasite to action.
In addition, being a cold-blooded animal, the tick clearly senses the infrared radiation of warm-blooded organisms, but for hunting it is still a secondary irritant.
Vaccination against tick-borne encephalitis for a child
One of the methods of preventing tick-borne encephalitis is vaccination. It is widespread in endemic areas (Ural, Siberia, etc.).
Its meaning is that after the vaccine is administered, the child develops immunity to the virus due to the formation of antibodies. If a child is bitten by an infected tick, infection will either not occur at all, or the disease will be mild.
If a tick bites a child, then vaccination is pointless. In the treatment of tick-borne encephalitis, immunoglobulins are used, and if a vaccine is administered, its constituent substances will impair the functioning of immunoglobulins.
In this case, vaccination is started no earlier than two weeks later. If parents want to protect their child and administer the vaccine in advance, there are two schemes:
- Standard (planned): two vaccinations with an interval of three months. Revaccination after a year, then every three years to maintain immunity.
- Emergency: 2 injections two weeks apart for those who move to endemic areas for tick-borne encephalitis due to business trips or for permanent residence.
You need to start routine vaccination in the fall, so that you can get the second shot in the spring. Immunity is developed only after 2-2.5 weeks. A child does not develop lifelong immunity, so revaccination must be carried out according to the schedule. The age at which this vaccination begins depends on the drug. The domestic drug is used from 3 years of age, imported - from one year. An injection is given subcutaneously in the shoulder area.
It is important that the planned vaccine does not overlap with others on the vaccination schedule. A pediatrician will help you plan the dates for introducing medications.
The tick-borne encephalitis vaccine has a number of contraindications:
- acute form of any disease (ARVI, acute respiratory infections, bronchitis, tonsillitis, etc.);
- intolerance to components and allergic reactions to the composition of the vaccine;
- if other vaccinations were given less than 2 months ago;
- allergy to chicken protein and/or chicken meat;
- serious pathological changes in the liver, kidneys, blood diseases, etc.;
- immunodeficiency states.
In any case, you should consult your pediatrician before vaccination. If there are contraindications, vaccination cannot be done!
Of course, there is a lot of debate about whether children should be vaccinated. Some people are afraid to do them because of possible side effects, including:
- skin rash;
- runny nose;
- redness of the skin in the injection area;
- temperature increase;
- loss of appetite.
Experts call such symptoms a normal reaction to the injected substance. But if the discomfort does not go away for a long time, you should consult a doctor.
Regarding vaccination against tick-borne encephalitis, it is important to understand that the disease itself is much more severe and has more consequences than ailments after vaccination. Moreover, the child may feel unwell after any vaccination.
Based on this, we can draw conclusions:
- Vaccination will help you survive tick-borne encephalitis in a mild form or not get it at all.
- The consequences after the injection may be in the form of ailments, but this is absolutely normal.
- Only parents are responsible for the health of their child, and they make the decision about vaccination: doctors can only recommend it.
As for tick-borne borreliosis , there is no vaccination against it. Once the diagnosis is made, treatment begins with antibiotics.
To sum up, we can definitely say that ticks are something to be wary of. The rules for visiting the forest in spring and early summer should not be neglected. Ideally, it is better to postpone such walks until persistently hot weather, when tick activity is zero. If you are planning a trip to a forest area, dress your child so that there are no exposed skin areas, and before doing so, treat the clothes with special aerosols.
If a child is bitten by a tick, do not panic. To avoid dangerous consequences, there are several home methods for removing it (and it is simply necessary to remove it) and ways to provide assistance. For prevention purposes, pay attention to vaccination. The vaccination itself is safe and minimizes the risk of tick-borne encephalitis.
How a tick clings and stays on the host’s body until it bites
When a person or animal passes through the grass where the tick sits, contact occurs and the parasite mechanically clings with its paws to the hair or clothing of the owner. Next, his most important task will be to find a favorable place for suction. Until this moment, the parasite must stay firmly on the integument and not be noticed (you need to protect yourself from the host’s defensive actions, such as shaking it off).
The tick clings so tightly to the body that it is almost impossible to shake it off. The only way to get rid of a tick before it attaches itself is to deliberately remove it from the surface of the body.
High efficiency of retention on the host’s body is achieved due to the special morpho-anatomical structure of the ticks’ body:
- the entire body of the parasite is covered with small spines and bristles, which increase friction and increase the likelihood of snagging;
- the legs have sharp paired claws - they cling tightly to the fabric, like small hooks (in highly specialized ticks, the diameter of the bend of the claw can coincide with the diameter of the victim’s hair, and then a kind of lock is formed, which is extremely difficult to disengage);
- some of the mites can bend the head section towards their body, like pinching the wool or fabric between the proboscis and the body with tongs;
- the body is flattened in the dorso-ventral direction, which complicates the task of crushing the parasite.
It is also useful to read: Symptoms that may appear in a dog after a tick bite
While the tick has not bitten, all these devices allow it to remain on the owner’s body for a long time, increasing the likelihood of successful feeding.
Given the size of the prey relative to the size of the tick, the arthropod often has to travel considerable distances, so selecting the location of the bite may take several hours. Since the tick drinks blood for a very long time (usually for several days), the process of choosing an attachment site is extremely important and takes a significant amount of time.
On a note
From the above, it becomes clear that the tick does not bite immediately. Between the time it hits a person and the time it bites, a significant period of time always passes. Therefore, if you examine yourself after walks in nature, you can avoid a parasite bite.
If the arachnid fell off at home
In a situation where the parasite bites a person and falls off after a few hours, it often goes unnoticed. A red spot, slight inflammation, and slight itching remain on the body. The tick falls off if it has fully satisfied its need for food and replenished its nutritional reserves.
Tick drunk on blood
If a thick tick falls off at home, there is no future for it. The nymph will not be able to continue development because there is no soil. The female will not be able to lay eggs for the same reasons. After some time, the parasite dies. The tick is dangerous if it has not drunk blood, then it can bite again. There is no need to worry too much about where the tick goes in the apartment. Even if he is not discovered, he will soon die.
Finding a place for suction and the initial stage of introducing the oral apparatus into the skin
Many species of ixodid ticks are characterized by certain attachment sites on the host's body where the parasites are found in the greatest number of cases, while in other places bites occur less frequently or are absent altogether.
Such a strict confinement to certain places on the victim’s body is explained by a number of reasons. Firstly, this is the exceptional importance of animals’ ability to self-clean: shaking, licking, gnawing, pecking and crushing parasites is used. Therefore, when attached to pets, ticks look for places where self-cleaning is most difficult: the ears, scruff of the neck, head, anal and groin areas.
Another important factor is the microclimate in the selected area of the victim’s body. Different areas of the skin have different temperatures and degrees of moisture, and the nature of secretions and acid-base balance also differ. The ideal place for the parasite to attach itself should not be constantly exposed to direct sunlight, otherwise the tick will quickly lose its water supply.
The actual structure of the skin is also important – how rough it is and how well vascularized it is.
On a note
In the case of wild animals, one should not lose sight of the factor of aggregation, that is, when there are many ticks on one host at once. In this case, some types of parasites choose areas distant from the place of attachment of others. Parasites form local accumulations, which significantly reduces the effectiveness of local immune reactions of the host organism and increases the efficiency of the ectoparasite's nutrition.
The sites of tick bites in humans have been well studied. Shoes and clothing limit the number of places for attachment, but ticks find a way out of this situation.
The largest percentage of ticks attached to a person occurs in the axillary region, then in descending order: on the chest, abdomen, groin, buttocks, and legs. In children, frequent attachment to the head is also observed. It is worth noting that ticks navigate perfectly under clothing, making their way to the body even through small cracks.
The structure of the parasite's mouthparts
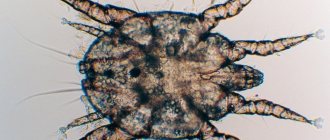
The oral apparatus of a tick is a complex formation and consists of several components, each of which has its own morphology and functions. You can examine some interesting nuances in detail under a microscope (see photo below):
The oral apparatus includes a base, a proboscis or hypostome, one pair of chelicerae embedded in cases, and a pair of palps. The base of the proboscis has the form of a capsule with a dense chitinous cover - here the ducts of the salivary glands pass and the pharynx begins. The palps have a segmented structure, consist of 4 segments and perform a tactile function.
The hypostome is an unpaired chitinous plate immovably attached to the base. It has the appearance of an elongated “sting”, on which a large number of hooks bent back are located in regular longitudinal rows, as shown in the photographs below:
Towards the top, the hooks become smaller, forming a crown of small and at the same time very sharp thorns. When a tick bites, the sharp hypostome is involved in cutting through the skin along with the chelicerae.
The back-directed teeth of the proboscis do not interfere with its penetration into the integument, but they prevent the reverse forcible removal of the attached tick, acting as an anchor. Therefore, in no case should a tick be forcibly pulled out of the skin with a sharp movement, as this risks that the proboscis (or even the entire head of the parasite) may remain under the skin, causing suppuration.
On a note
At the base of the hypostome a pair of chelicerae are attached, which look like sharp blades enclosed in cases. Chelicerae are very mobile and can cut through the skin and integument at different angles and to different depths. When at rest, they are enclosed in cases that protect them from mechanical damage.
Collectively, this is called the gnathosoma and represents the anterior section of the tick’s body, which, during a bite, plunges into the integument of the victim’s body.
How does a tick bite?
After finding a suitable place to feed, the parasite begins to dig into the skin.
When a tick bites, it cuts through the upper stratum corneum of the skin, making alternating movements with its sharp chelicerae. This is similar to how a surgeon wields a scalpel (only the parasite has two of them at once).
Despite the high mechanical strength of the upper layer of skin, it does not create serious obstacles to the path of the tick's oral organs to the inner layers where the blood vessels are located. Moreover, there is no direct relationship between the thickness of the skin of the preferred host and the length of the chelicerae.
It is also useful to read: The first symptoms after a tick bite in a person
The process of cutting through the skin lasts the first 15-20 minutes from the moment the bite begins.
At the same time, the process of inserting the proboscis into the incision formed by the chelicerae begins. The entire proboscis is completely immersed in the wound, almost to the base of the head, and the palps are bent almost parallel to the skin.
As a result, the length of the gnathosoma quite accurately reflects the depth of penetration of the tick into the integument - during a bite, the parasite penetrates quite deeply, and the gnathosoma is located in the middle layer of the skin, rich in blood vessels.
On a note
An important fact is that the tick is able to regulate the depth of penetration of the proboscis into the integument. This depends on the size of the victim and the thickness of its skin. It is also worth considering that the deeper the tick burrows into the skin, the stronger the host’s immune defense reaction will be. Severe inflammatory processes may begin, negatively affecting the tick and reducing the chances of successful feeding.
Scientists also noticed that species that are characterized by frequent changes of hosts penetrate to a shallower depth, as this minimizes the chances of injury to the parasite’s gnathosoma and increases the likelihood of the success of the next feeding.
Thus, the entire stage of the bite itself (suction) lasts quite a long time - usually this requires at least half an hour. All this time, anesthetic substances are injected into the wound, so the victim does not experience any unpleasant sensation or pain (along with saliva, anticoagulants and some other substances are also injected). As a rule, it is possible to find out about a bite only when a parasite is detected on the body.
Next, the tick’s feeding process occurs, a step-by-step description of which is given below.
Parasite feeding process
After the tick has successfully burrowed into the skin, it begins to feed. At this moment, along with the proboscis, the wound also contains chelicerae with sheaths that expand the tissues near the hypostome.
Directly from the skin, the proboscis is separated by a special cement case, which represents the frozen secretions of the parasite's salivary glands. This case has the shape of a tube and extends into the skin a little further than the top of the proboscis.
Accordingly, first the food enters the cavity of the case, and then into the pre-oral cavity of the tick. On the surface of the skin, this case ends in a frozen roller, to which the base of the proboscis is glued.
This is interesting
After a bite, the tick is retained in the host not only thanks to the hooks of the proboscis, but also due to the outgrowths on the cheliceral cases, which appear to be sealed into the walls of the cement case. This feature increases the reliability of attachment and protects the tick’s oral organs from inflammatory infiltrate while the parasite drinks blood.
It is worth noting that the tick feeds not only on blood, but also on lysed skin tissue where the proboscis is inserted.
After the parasite has formed a cement sheath and is finally established, the process of blood absorption begins. There is an opinion that ticks prefer a certain blood type, but this is not true. Blood type has nothing to do with the choice of victim or saturation - ticks equally often bite people with different blood groups.
At the blood-sucking stage, anticoagulants are introduced into the host tissue, which prevent blood clotting, so that the parasite can feed for a long time. Additionally, digestive enzymes from saliva are injected into the wound, and partial dissolution of the adjacent tissue occurs. Because of this, a local inflammatory process forms in the host’s body, which in some cases can spread and cause an increase in the victim’s temperature.
This is also dangerous because pathogens such as Lyme disease and tick-borne encephalitis can enter the host’s body along with the tick’s saliva. Moreover, the longer an encephalitic or borreliosis tick feeds, the greater the amount of saliva it produces and the greater the likelihood of infecting a person with the corresponding disease.
The duration of tick feeding varies and depends on the stage of its ontogenesis and gender. Nymphs drink blood for 2-3 days, and sexually mature females can stay on the host’s body for up to a week. Males usually do not feed, and if a male does attach itself, it stays on the host for only a few hours.
Prolonged feeding of females is associated with a clear dependence of the success of egg development on the degree of saturation of the parasite. Only a completely well-fed female can fully ripen eggs and lay them. Therefore, female ticks are the most active and dangerous to humans.
On a note
It is quite easy to distinguish a female tick from a male. The male has a wide chitinous matte scute on the upper side of the body, which completely covers the back, while in females the scute only reaches the middle of the back.
Tick nymphs become saturated relatively quickly. They need food for molting and further development, but they are also carriers of pathogens of various diseases, like adults.
The body sizes of a well-fed and hungry tick differ significantly - they can increase 25 times! And even if it was not immediately possible to notice a tick bite, then after it has been on the body for some time, it is difficult not to notice the parasite, since it becomes much larger (a engorged tick looks like a gray sac or a grape).
The increase in body size of the parasite during blood sucking occurs unevenly. During the first day after attachment to the host, the size of the tick's body does not increase, but even decreases slightly, as significant evaporation of water occurs. The second stage is the longest, with the size of the tick increasing 10-20 times.
After the tick is completely saturated, it disappears on its own. The muscles of the oral apparatus relax, the chelicerae are pressed tightly against the proboscis, and the tick easily removes it from the integument of the victim’s body.
After falling away from the host, the parasite again becomes free-living for some time - it looks for a favorable place in its natural biotopes (forest, park, square) and lays eggs, preparing for molting and wintering. It no longer has contact with its previous host - its function is completed, and the next stage of the parasite’s life cycle begins.
Effective treatments
To treat unbearable itching on human skin after bed tick bites, medications and traditional medicine can be used.
Medications
If you suspect an autoimmune reaction to a dust mite bite, you should first visit an allergist who will prescribe appropriate treatment.
Medications to treat dust mite allergies:
- nasal drops and sprays;
- antihistamines.
The doctor may also prescribe corticosteroids if the allergy has become advanced.
When taking medications, you must remember that they only temporarily relieve allergy symptoms. To completely eliminate an allergen, you need to fight it.
Nasal drops and sprays:
- Aquamaris - solution for rinsing the nose;
- Tizin Alergy - nasal drops help relieve allergic rhinitis;
- Reactin - spray quickly relieves allergy symptoms;
- Vibrocil, Nazivin.
For domestic tick bites, the patient is also prescribed eye drops.
Antihistamines
Tablets, nasal sprays, and eye drops are used to treat allergies. In some cases, antihistamines are administered intramuscularly.
Currently, there are 4 generations of effective allergy medications. They are not addictive, perfectly relieve symptoms and reduce the risk of side effects. Medicines are actively used to treat dust mite allergies.
First generation drugs
Sedative medications have a strong effect, but have contraindications for use. The effect of the drugs lasts 6 hours.
This:
- Tavegil;
- Diphenhydramine;
- Fenkarol;
- Suprastin;
- Pipolfen;
- Meclizine.
First generation drugs are used to treat allergic reactions that cause difficulty breathing.
II generation drugs
This group of medications includes non-sedative medications.
Their use is recommended for skin itching and dermatitis:
- Trexil;
- Gistalong;
- Fenistil;
- Levocetrizine;
- Claritin;
- Zodak.
These drugs have a cardiotoxic effect and are therefore contraindicated for people with heart and vascular diseases.
III generation drugs
Medications are characterized by effective antihistamine properties:
- Zyrtec;
- Erius;
- Telfast.
III generation drugs are valued for their lack of side effects. They are often prescribed to treat allergies to dust mites.
The medications eliminate dermatitis, reduce asthma symptoms, and do not have a toxic effect on the cardiovascular system.
IV generation drugs
The most harmless medicines, however, are contraindicated for children and pregnant women.
These include:
- Bamipin;
- Desloratadine;
- Xizal;
- Levocetirizine.
The drugs do not make you sleepy and do not affect the heart.
Folk remedies
Traditional medicine recipes help cope with allergic rashes on the body as a result of a bed tick bite.
Here are some popular methods:
- St. John's wort lotions help relieve itching. Preparation of infusion: 1 tbsp. crushed raw materials are poured into a glass of boiled water and left to infuse. Soak a cotton pad in the prepared product and apply it to the damaged area for half an hour.
- Effective medicinal herbs are calendula and chamomile. Lotions are also prepared on their basis.
- Places of dust mite bites on the human body should be wiped with a cotton pad soaked in pure vinegar.
- Luda cubes and tea bags help remove the tooth.
- Bite areas can be treated with plantain juice and aloe. Treatment is carried out several times a day. The juice of medicinal plants has an antibacterial effect.
- Toxins accumulate in the body. To remove them, it is recommended to drink several tablets of activated carbon.
- Onions and garlic will help scare off bloodsuckers. If you mix the juice of these plants together and apply it to the wound, the itching will decrease and rashes on the body will become less noticeable.
Essential oils of lemon, lavender, orange, wormwood, and juniper help with bites. Oils of pine needles, mint, and geranium are also effective.
Traditional recipes help cope with the manifestations of allergies at an early stage; if the process is started, it is recommended to use medications.
A few words about what to do if a tick has already attached itself
As noted above, due to the substances contained in the saliva of the tick, a person or animal does not feel the bite of the parasite. Often people notice a tick on their body only when it has already attached itself and started feeding.
In any case, it should not be pulled out by force from the skin, much less try to crush it. Incorrect actions can lead to additional portions of infected saliva getting into the wound, and the head of the parasite will come off the body and remain in the wound (this will cause suppuration in the future).
The attached parasite must be removed without undue delay, but as carefully as possible. You can do this yourself - there are several ways to properly remove a tick from a wound (see other articles on the site). If the bite occurred in a region that is potentially dangerous from the point of view of infection with tick-borne encephalitis or borreliosis, then the tick should be tested at the appropriate medical institution. If pathogens of a particular disease are identified in the parasite, doctors will give further recommendations - amateur activities here can already be dangerous.
We should not forget about preventive measures. After walks, you need to carefully examine yourself, children and animals, and before going out into nature, use repellents, wear closed clothes and shoes. With the right approach, it is almost always possible to remove a tick from clothing (or body) in time - long before it has time to attach itself.
Video recording of a tick bite at high magnification - all the details of the process are visible
First alarming symptoms
Symptoms of Lyme disease.
As mentioned earlier, the first symptoms of tick-borne encephalitis and Lyme disease do not appear immediately: on average, 2 weeks after the bite. You should immediately contact your pediatrician if your child has:
- fever, increased body temperature;
- weakness, lethargy, drowsiness;
- headache;
- loss of appetite;
- nausea, vomiting;
- red rash on the body;
- disorders of consciousness;
- paresis of the limbs (decreased muscle strength).
The tick-borne encephalitis virus first enters the child’s blood through a bite, then it spreads throughout the body through the bloodstream: first to the lymph nodes, internal organs, then to the brain and spinal cord. When the amount of virus in the blood increases (viruses divide multiple times and increase in number), the first symptoms appear.
As for Lyme disease , the first symptom is a rash on the body (redness of various diameters - from 0-60 cm). There may be no other symptoms at first. Parents, when they see such red spots, turn to allergists or dermatologists, assuming that this is an allergic reaction or dermatitis. But if two weeks ago (or even a month ago) there was a tick bite, we can assume that the child is developing tick-borne borreliosis.
Tick bites are dangerous, so at the first such symptoms you need to consult a doctor: the hospital will conduct a blood test, identify the cause of the child’s poor health and prescribe therapy. You should not put off visiting the pediatrician and treat the symptoms like a common cold, as improper treatment will aggravate the situation and time will be lost.